THIRTY-THREE-YEAR-OLD Precious Tsindikeni from Muzarabani in Mashonaland Central province breaks down whenever she sees the bag of clothes she had prepared for her unborn child.
She was expecting to give birth in August this year.
However, she went into labour earlier than anticipated in early July while visiting her sister in Harare for a family emergency.
The early labour and subsequent loss of her baby left her emotionally scared, struggling to cope with the heartbreak of losing her unborn baby.
“I knew that my delivery date was approaching since my expected date of delivery was around August, but I had to rush to Harare for a family emergency,” Tsindikeni said.
But things did not go as planned.
This is the sixth part of the series, The high cost of motherhood: A silent maternal healthcare epidemic in Zimbabwe, supported by the International Women’s Media Foundation.
Painful reality
- Mater Dei undergoes huge transformation
- Mater Dei undergoes huge transformation
- Mental Health: Motherhood and mental health
- High cost of motherhood: A silent maternal healthcare epidemic
Keep Reading
On July 6, 2024 at around 7pm, Tsindikeni exprienced labour pain and was rushed to Sally Mugabe Central Hospital, one of the public referral maternal health institutions in the country which offers free maternal healthcare.
Sally Mugabe Maternal Hospital is part of Sally Mugabe Central Hospital, located in the medium-density suburb of Southerton in Harare.
Sally Mugabe Hospital, a vital healthcare institution in Zimbabwe, primarily serves low-income patients. Over the years, the hospital has become increasingly overwhelmed, particularly in its maternal care unit.
The influx of expecting mothers seeking affordable and accessible maternal healthcare has put a strain on the hospital’s resources and staff.
“When I got to the hospital at around 8pm, I was told that I was at 2 centimetres and I was taken to the waiting ward, where other expecting mothers were sleeping on the floor and I had to join them,” Tsindikeni narrated her ordeal to NewsDay.
At around 5pm during regular check-ups on the next day, Tsindikeni was told that her baby had passed meconium before delivery and she had to go for an emergency operation.
Meconium is the term used for a baby’s first stool, which can sometimes be passed before birth.
“I was then transferred to the early labour ward while the doctor told his juniors to book me for an emergency Caesarean section procedure at 4am.
“The doctor advised me not to push because it was not safe for the baby and I complied. However, I spent the whole night in severe labour pain.
“Before 4am, a female doctor attended me just before I went to the theatre and realised that the baby was close.”
She said she was helpless and confused about what to do as the doctor who attended her earlier “had been harsh on me”.
“She harshly commanded me to go back to the bed and to push. It took me almost 20 minutes to deliver, unfortunately, the baby couldn’t make it,” Tsindikeni said with tears rolling down her cheeks.
She was told the baby may have experienced foetal distress.
She struggled to come to terms with the devastating news of her baby’s death.
Since then, she has been grappling with the trauma of losing her first child shortly after birth and she is failing to move past the heart-breaking loss.
Tsindikeni is one of the mothers in Zimbabwe whose childbirth experience has left them with lifelong scars.
The trauma of her ordeal is a stark reminder of the challenges faced by countless women in the country.
Despite the joy and anticipation that typically accompanies the arrival of a new baby, Tsindikeni’s experience was marred by complications and heartbreak.
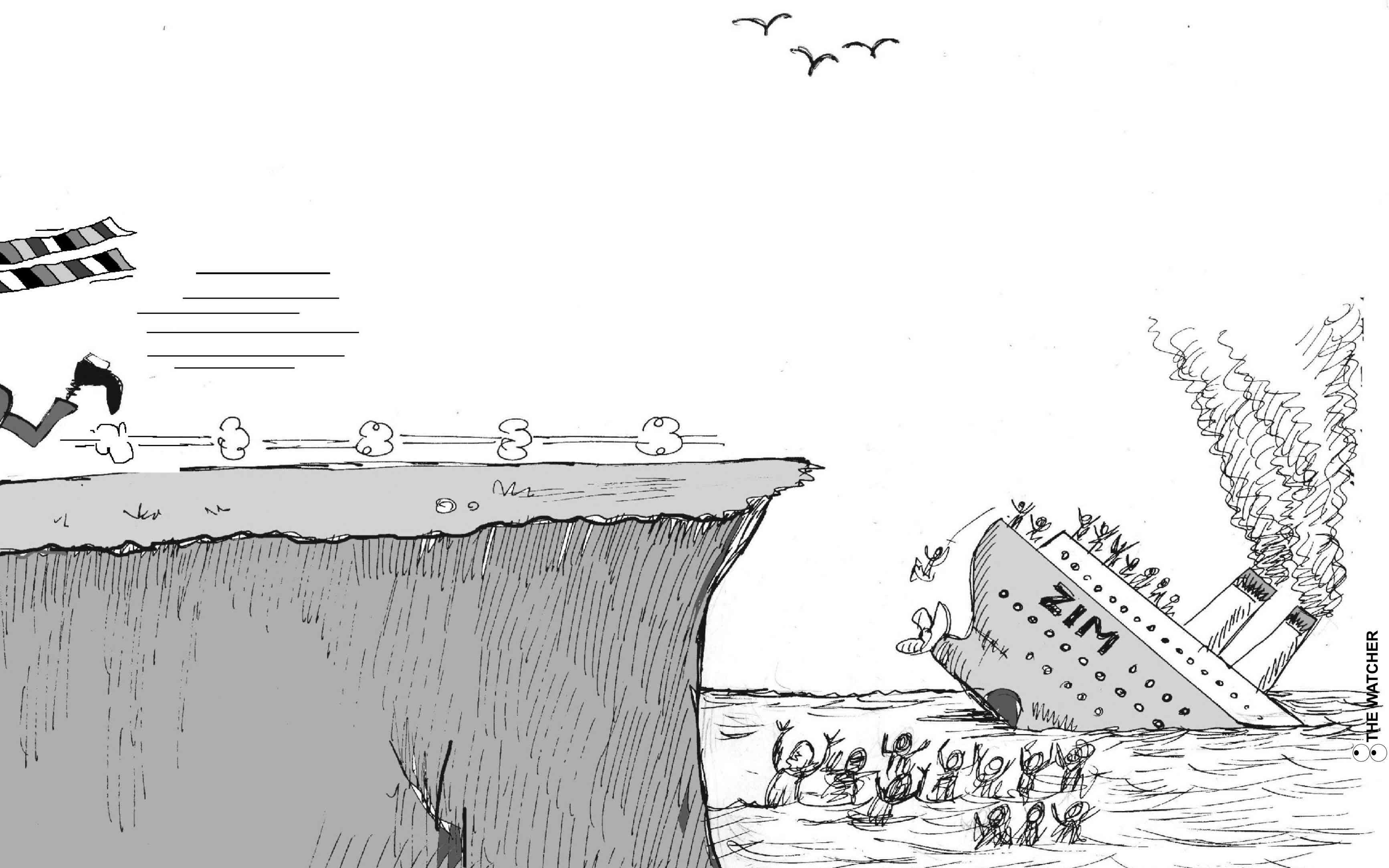
The maternal mortality rate remains high in the country, according to the Zimbabwe Coalition on Debt and Development (Zimcodd), a socio-economic justice coalition.
The National Development Strategy 1 emphasises the importance of quality healthcare services.
However, the country’s maternal mortality rate stands at 363 per 100 000 live births.
This is higher than the sustainable development goal (SDG)'s 3,1% target, which aims to reduce the maternal mortality ratio to less than 70 per 100 000 live births by 2030.
“This is worrying as the maternal mortality rate is considered a primary and important indicator of the country’s overall health status or quality of life,” Zimcodd said.
Tsindikeni believes the health sector has failed her despite prividing free maternal care as service is poor due to incapacitation.
“Up until now, I am heartbroken. I believe if they had taken me to C-section earlier, my baby could have been saved,” she said.
Tsindikeni lamented the fact that she could not afford private healthcare services, but vowed that in the future, she will save enough money so that she will not set foot at a public institution again.
Melody Chikanga***, a 21-year-old mother of a three-month-old baby from Epworth, a peri-urban community in Harare, describes her childbirth experience as a mixed bag of joy, pain and lost hope.
A giant in the room
Chikanga endured prolonged labour due to delayed medical attention.
“Although I managed to deliver my baby, the process left me with a severe vaginal tear which I believe could be obstetrics fistula,” she said, highlighting the physical and emotional trauma she continues to endure.
The UNFPA describes obstetric fistula as one of the most severe and tragic childbirth injuries which is a condition of having a hole between the birth canal and the bladder and/or rectum, often resulting from prolonged, obstructed labour without timely, high-quality medical intervention.
Women and girls affected by fistula experience leakage of urine, faeces or both, leading to chronic health issues, depression, social isolation and worsening poverty.
An estimated half a million women and girls in sub-Saharan Africa, Asia, the Arab States, Latin America and the Caribbean are living with fistula, with new cases emerging each year.
Despite being almost entirely preventable, the persistence of fistula highlights significant inequities and global inequality, underscoring the failure of health and social systems to protect the health and human rights of the most vulnerable women and girls. Zimbabwe is one of the affected countries due to its deteriorating healthcare system.
Poor maternal health care service
Health and Child Care ministry spokesperson Donald Mujiri said maternal delays would be attributed to various factors, including limited access to healthcare, inadequate resources and socio-economic barriers.
“However, addressing these challenges is crucial to preventing obstetric fistula and ensuring safe and quality maternal healthcare in Zimbabwe,” he said.
Over the years, the Health and Child Care ministry has faced several challenges in combating obstetric fistula, including limited resources, inadequate funding, equipment and infrastructure that hinder the provision of quality maternal healthcare and fistula repair services.
“Shortage of skilled healthcare providers and insufficiently trained healthcare providers, particularly in rural areas, exacerbate the shortage of skilled birth attendants and fistula repair experts,” Mujiri said.
He said the ministry was working with different stakeholders to introduce several initiatives aimed at reducing the incidence of obstetric fistula and improving the lives of women and girls in Zimbabwe.
“Currently, we are providing free obstetric fistula repair surgeries in collaboration with partner organisations like UNFPA, Fistula Foundation and Artmedis International,” he added.
***Not her real name